? ? ? SSI不僅會(huì)對患者的身體健康產(chǎn)生很大的影響�,也會(huì)額外增加醫(yī)院的醫(yī)療費(fèi)用支出���。以下為美國醫(yī)院發(fā)生的SSI在這兩方面所產(chǎn)生的影響�。
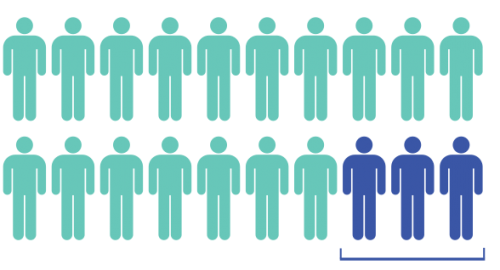
在腹部手術(shù)當(dāng)中����,每20例患者中就有3例SSI高發(fā)生率的風(fēng)險(xiǎn)。

? ? ?研究表明�,在腹部手術(shù)當(dāng)中���,每20例患者中就有3例SSI高發(fā)生率的風(fēng)險(xiǎn)[1-3]。
de Lissovoy G[4]等人對患者的住院天數(shù)進(jìn)行調(diào)查分析�����,結(jié)果發(fā)現(xiàn)SSI患者平均住院天數(shù)為15天����,無SSI患者平均住院天數(shù)僅為8天。SSI患者再次入院率為27.8%��,無SSI患者再次入院率僅為6.8%[5]���。SSI患者ICU入住率為29%�����,無SSI患者ICU入住率僅為18%���,相較于無SSI患者,SSI患者死亡風(fēng)險(xiǎn)增加了2倍[6]�����。
 ? ? ? ? ? ? ? ? ? ? ? ? ? ? ??
? ? ? ? ? ? ? ? ? ? ? ? ? ? ?? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ?
? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ?
? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ? ?
每年因SSI的花費(fèi)為100億美元 ? ? ? ??每例SSI患者額外費(fèi)用19000美元 ? ? ? ? ??每個(gè)醫(yī)院每年支付500萬美元的罰款 ? ? ? ? ? ? ??醫(yī)院負(fù)面影響
?
? ? ? 美國疾病預(yù)防控制中心報(bào)道,每年因?yàn)镾SI支出的醫(yī)療費(fèi)用100億美元[7]����;根據(jù)2009年和2011年的數(shù)據(jù)分析,每例SSI患者因SSI額外的醫(yī)療費(fèi)用支出為19000美元[5,8]�;每個(gè)醫(yī)院由于SSI每年需要支付500萬美元的罰款[9]。不僅僅是這些額外醫(yī)療費(fèi)用的支出���,SSI還會(huì)給醫(yī)院帶來較大的負(fù)面影響。
參考文獻(xiàn):? ? ?
1?Watanabe A, Kohnoe S, Shimabukuro R, et al. Risk factors associated with surgical site infection in upper and lower gastrointestinal surgery.?Surg Today.?2008;38(5):404-412.
2?Wick EC, Vogel JD, Church JM, Remzi F, Fazio VW. Surgical site infections in a "high outlier" institution: are colorectal surgeons to blame??Dis Colon Rectum.?2009;52(3):374-379.
3?Sutton E, Miyagaki H, Bellini G, et al. Risk factors for superficial surgical site infection after elective rectal cancer resection: a multivariate analysis of 8880 patients from the American College of Surgeons National Surgical Quality Improvement Program database.?J Surg Res.?2017;207:205-214.
4?de Lissovoy G, Fraeman K, Hutchins V, Murphy D, Song D, Vaughn BB. Surgical site infection: incidence and impact on hospital utilization and treatment costs.?Am J Infect Control.?2009;37(5):387-397.
5?Wick EC, Hirose K, Shore AD, et al. Surgical site infections and cost in obese patients undergoing colorectal surgery.?Arch Surg.?2011;146(9):1068-1072.
6?Kirkland KB, Briggs JP, Trivette SL, Wilkinson WE, Sexton DJ. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs.?Infect Control Hosp Epidemiol.?1999;20(11):725-730.
7?Scott RD. The Direct Medical Costs of Healthcare-Associated Infection in US Hospitals and the Benefits of Prevention.?Centers for Disease Control and Prevention; March 2009.
8?Tanner J, Khan D, Aplin C, Ball J, Thomas M, Bankart J. Post-discharge surveillance to identify colorectal surgical site infection rates and related costs. J Hosp Infect. 2009;72(3):243-250.
9?Rau J. Latest Hospital Injury Penalties Include Crackdown On Antibiotic-Resistant Germs. 2016; https://khn.org/news/latest-hospital-injury-penalties-include-crackdown-on-antibiotic-resistant-germs/._Accessed January 29, 2018.